- Home
- About
- GI Diseases
- Patient Education
- Gallery
- Contact Us
- Blog
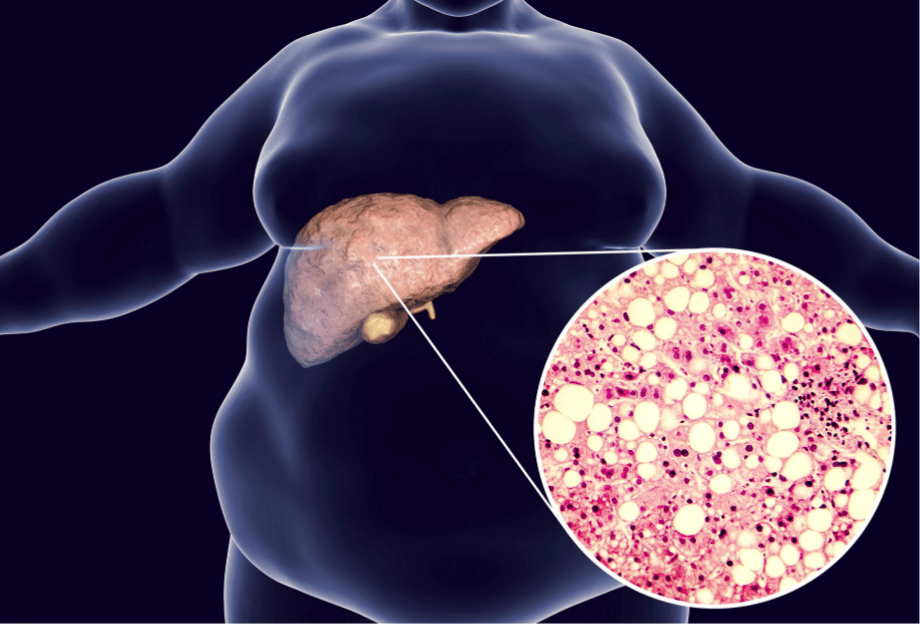
- Fatty Liver Treatment in Hyderabad
- Laparoscopic Inguinal Hernia Surgery in Hyderabad
- Best Laparoscopic Gallbladder Stone Treatment in Hyderabad
- Best Pancreatic Cancer Treatment in Hyderabad
- Gastric Cancer Treatment in Hyderabad
- Colorectal Cancer Treatment in Hyderabad
- Liver Cancer Treatment in Hyderabad
- Acute Pancreatitis Treatment in Hyderabad
- Gallbladder Cancer Treatment in Hyderabad
- Chronic Pancreatitis Treatment in Hyderabad
- Blood Vomiting Treatment in Hyderabad
- Liver Cirrhosis Treatment in Hyderabad
- Blood in Stool Treatment in Hyderabad
- Alcohol Consumption Cause Gastrointestinal Cancer
- Best Constipation Treatment in Hyderabad
- Tips for Chronic Constipation Relief Dietary and Lifestyle Changes
- Dietary Management of Irritable Bowel Syndrome
- Irritable Bowel Syndrome Treatment in Hyderabad
- Hepatitis B Treatment In Hyderabad
- Best Doctor for Gas (Flatulence) in Hyderabad
- Obesity and gastrointestinal cancers: a full guide everything you need to know
- Best Anal Fissure Treatment in Hyderabad
- Best Piles (Hemorrhoids) Treatment in Hyderabad
- Perianal Abscess Treatment in Hyderabad- Dr. K.V Dinesh Reddy